Afsal realised he had run out of soap. As always, he approached Chandran, the local shopkeeper for his usual brand of soap. But this time, the response took Afsal by surprise.
“You can’t have that brand,” said Chandran, “I will give you this instead, it is made by another company.”
Chandran showed him a soap he’d never seen before.
“But why can’t I have the brand that I have always used?” asked Afsal. “Besides, changing soaps gives me skin problems.”
“I hate to tell you this, Afsal. Maybe you weren’t reading the news; you should know that you have no choice in the matter anymore. It is now my job to pick the soap brand for you. Come on - you know all soaps contain the same ingredients.”
Now frustrated, Afsal asked the shopkeeper: “What’s going on? What about my cooking oil, my toothpaste, my underwear? Can I choose the brand I want?”
Amused at the extent of Afsal’s ignorance, Chandran explained: “Same thing. You can tell me what item you need, whether it is soap, toothpaste, even underwear. Still, I get to pick the brand for you.”
Leaning closer, he whispered in Afsal’s ear: “Did you know that I can now sell you the brand that gives me the biggest margin? You might even think it is cheaper than your favourite brand, but what you probably don’t know is that I paid much less to buy that product, than your brand. But don’t tell anyone that.”
Read: Everyday Health | Hepatitis A, the friendly neighborhood jaundice
Everyday Health | Wheelchairs don’t climb stairs: What society can and should be doing for the differently abled
In other words, Afsal the customer had no choice any more. Chandran the shopkeeper could sell the customer any brand, and that choice was largely determined by the profit from that sale. The profit obviously was the difference between the price he paid to buy the soap from the stockist, and the price he charged Afsal. It turns out that for less popular brands, the profits (margins) are generally greater.
What does this story represent?
As absurd as this fictional story might seem, it describes a present-day problem: several recent directives from the government and Medical Council of India have asked doctors to use generic names of medicine on their prescriptions, instead of brand names. While these directives might seem well-intentioned at first glance, they bring along with them some serious problems.
Also check: Everyday Health: Excessive honking can be bad for your heart | Video
The foremost objection with the directive is that taking away the doctor’s right to choose the appropriate brand for the patient will simply allow the medical shop or pharmacy to dispense whatever brand they wished to.
In the story above, Afsal the customer represents the doctor who prescribes a medicine, while the shopkeeper represents the pharmacy which would dispense the medication after receiving the doctor’s prescription. The doctor has just lost his right to choose which brand of medication he could write for his patient, and the story explains the consequences.
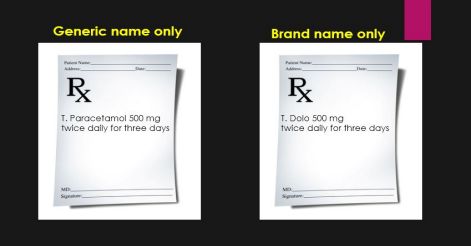 The difference between generic and brand name prescribing. In India, there are 368 companies that manufacture paracetamol, under over 800 brand names. Unfortunately, not all brands have the same quality.
The difference between generic and brand name prescribing. In India, there are 368 companies that manufacture paracetamol, under over 800 brand names. Unfortunately, not all brands have the same quality. What is the need for this article?
The problem of generic prescribing is complex. Many superficial comments and views have recently been made on this topic - much like the case of the blind men who met the elephant for the first time, each person seeing the problem from only his or her perspective.
For instance, centres of excellence might have the privilege of selecting and stocking medications of the highest quality in their pharmacy. Doctors who work in such places need not worry about what brand to prescribe. Just as in western nations, these doctors can safely prescribe the generic name, and the pharmacy will ensure that the patient receives medication of good quality.
This is not the case however for the vast majority of doctor-patient encounters in India, where most patients obtain their medicines from a local clinic or medical shop. The real question is whether this medicine contains the promised ingredient in the right amount, which will actually relieve his or her suffering.
This article examines the ground reality of prescribing, explains the terminology, and offers some practical solutions. It was written after receiving input from patients, doctors, nurses, pharmacists, hospital administrators, pharmaceutical company employees, industry experts, drug stockists, pharmacologists, media, government officials, drug inspectors and several others.
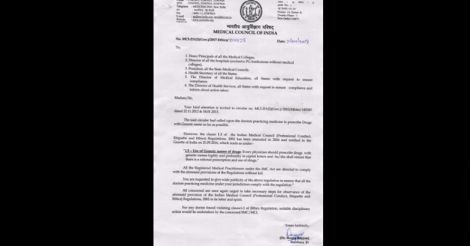 Doctors want the patient to get better, and generally prescribe the brand of medicine that they can trust, from experience. A recent circular from the Medical Council of India has however stated that doctors should prescribe drugs using generic name. Although at this time, the notification does not technically prohibit doctors from using a brand name, the wording has caused concern among doctors.
Doctors want the patient to get better, and generally prescribe the brand of medicine that they can trust, from experience. A recent circular from the Medical Council of India has however stated that doctors should prescribe drugs using generic name. Although at this time, the notification does not technically prohibit doctors from using a brand name, the wording has caused concern among doctors. What does ‘generic name’ and ‘generic medicine’ mean?
Generic name refers to the name of the main active chemical ingredient in the tablet or injection. It remains the same regardless of who manufactures it.
For example, the commonly used pain reliever paracetamol is manufactured by 368 different companies in India. Each company gives their paracetamol tablet a different brand name, such as Calpol, Crocin, Dolo, Paracip etc. Though the names are different, each of these products contain exactly the same active ingredient, that is paracetamol. Each brand name is owned by the particular manufacturing company, which indicates to the customer that the product was manufactured using the standards established by that particular company.
Each pharmacy or medical shop might stock a few of these brands based on their preferences and local prescribing pattern.
If paracetamol tablets are produced without such brand names attached, it is called generic paracetamol. It is somewhat similar to a mobile phone or a refrigerator that does not have a manufacturer’s label or other specific identifying information printed on it.
When a doctor is asked to write only the generic name, he writes ‘Paracetamol’ instead of ‘Dolo’, ‘Calpol’ or ‘Crocin’.
In reality, however, when the doctor writes the generic name ‘Paracetamol’ on the prescription , the medical shop salesperson will choose from one of the brands of paracetamol he has in stock and then dispense.
Even if the doctor wrote the preferred brand on the prescription, it is commonplace for the person at the medical shop to ask the patient: “We don’t carry this. Shall I give you the same medicine made by a different company?” and then switch to the shop owner’s brand of choice.
How is a medication tablet made?
Each tablet contains an active ingredient, for example paracetamol, in a given dose. But the bulk of the tablet is composed of filler material, which may be starch derivatives, gelatin or other. In other words, all of what we see as the tablet or capsule is not medication.
These materials bring stability to the tablet, the purpose being to release its active ingredient in the gut, to be absorbed into the bloodstream and eventually delivered to tissues and cells - at the optimal concentration and timeframe.
An improperly manufactured tablet might not contain the dose specified of the active ingredient; some counterfeit tablets contain no medication at all. In addition, medications need to be packaged carefully and often require to be stored in a cool dry place. When exposed to hot or humid conditions, the chemical constituent can get altered, rendering it useless or potentially harmful.
Thus, the quality of medication that reaches the patient not only depends on the quality of the manufacturing process, but also the packing, transport, storage and the duration it sits on the shelf.
Commonly used terms
1. Generic generic: Essential medications such as paracetamol that are manufactured with no brand name attached. The package will only have ‘paracetamol’ printed on it. These are manufactured by several companies, big and small. Some large companies sell the same medicine under their brand name too.
2. Branded generic: Medications whose patent has expired, and can be made by any licensed pharmaceutical firm, who will give the product a unique name of their choice. Frequently, medicines, once successful, become known by these brand names. The package will have both the brand name and the generic name printed on it: for instance, ‘Dolo’ or ‘Calpol’ are brand names, while “Paracetamol” is the generic name.
3. Branded (original): Very few medicines are in this category. These are medicines that are patented, and can only be manufactured and sold by the company that invented it - until the patent expires.
Why are popular brands more expensive?
To illustrate this with an example, consider the difference between an umbrella we buy from the pavement vendor for Rs 30 and an umbrella purchased for Rs 350 from the outlet store of a well-known brand. One might wonder, aren’t all umbrellas the same?
Obviously, though the cheap umbrella will work for some time, it develops leaks faster, gets inverted in the wind, gets stuck and eventually lasts less than the more expensive umbrella.
When a customer pays Rs 350 for a popular brand umbrella, all of that money is not exactly used to buy cloth and metal. A substantial part of that amount is used to set up and maintain state of the art factories, staff training, quality control, advertising, taxes, licenses and so on.
In contrast to cheap companies, reputed makers of any product – ranging from drugs, apparel, umbrellas, mobile phones or cars - pump more money into research and development (R&D). They use more automation, reducing the chance of error. They invest generously in improving the reliability of their product, which translates into customer loyalty.
In other words, while buying the branded umbrella, the customer is not only buying the physical product, but its reputation and trustworthiness. The money paid helps the company to maintain its high standards, in addition to generating profits.
In the field of pharma, branded generics are cheaper than original brands because the cost of product development (R&D) has already been recovered by the parent company before the medication went generic. Generic generics are even cheaper because there is no advertising involved.
What else determines the selling price or MRP of a medication?
Apart from the cost of production, what really pushes up the final selling price of a medication is retail mark-up.
If a tablet actually cost 10 rupees to produce including the manufacturer’s profit, the final selling price, or MRP (maximum retail price) at the medical shop could be 30-70% higher at Rs 13-17. This difference of Rs 3-7 is called retail mark-up. This add-on cost includes operating cost of transportation, storage, and dispensing medicines, in addition to profit margin for the stockist and retailer.
If a particular brand’s retail mark-up is 30%, traditionally 10% goes to the stockist and 20% goes to the retailer or medical shop. Much higher mark-ups also occur, as in the case of certain cancer medicines.
Thankfully, a cap on retail mark-ups has been put in place for 348 essential drugs by the Drugs Price Control Order of 2013. This order requires that the ceiling cost of a medicine is based on average market price, and caps off the maximum margin to the retailer at 16%.

Isn’t cheaper medicine better for the patient?
Some less-known brands might work out cheaper for the patient, as the MRP will be lower than established brands. However, when to comes to margin or profit, less known brands score big for the pharmacy. This is because the difference between buying price (cost price) and selling price (MRP) will be greater, and some companies provide special incentives to the pharmacy such as ‘buy one box, get one free’ and so on. As the margin is huge, some pharmacies even offer a ‘discount’ while dispensing such brands, which keeps the patient happy.
The patient however does not realise that the product could have been purchased at a throwaway price from a relatively unknown, low-quality manufacturer. In some cases, the tablet might not contain the right amount of medication listed, or could have been made in unhygienic and damp environment, stored at unacceptably warm and humid conditions, damaging the chemical ingredient within. As a result, the patient might not experience the desired benefit from the tablet.
The Chhattisgarh sterilisation camp tragedy of 2014 that took the lives of thirteen women was a direct consequence of using cheap and substandard medicines.
 Representational image
Representational imageWhy are doctors being asked to prescribe in generic format?
With the number of pharma companies mushrooming to well over 10,000, the number of brands available in India is over 110,000 and the average pharmacy stocks about 2000 of them. It can be difficult for the pharmacy staff to familiarise with and then correctly identify each brand. One must keep in mind that another pharmacy in another location will have yet another 2000 brands that reflects the local prescribing pattern of doctors.
There being only 26 alphabets in the English language, many brands end up with similar spellings or may phonetically sound the same. Doctors’ handwriting may be the butt of several jokes. However, when an illegibly written prescription gets read wrong by the pharmacy staff, it is no longer funny. This increases the chance for error while dispensing; the patient could end up consuming the wrong medicine. To reduce the risk of such errors, many doctors have already switched to writing prescription in capitals, and lately, to electronic prescribing.
Considering all of this, if the doctor were to prescribe generic name, it becomes easy for the pharmacy staff to correctly service the patient. It also makes it easier for other doctors to know what the medicine prescribed is, especially if the brand prescribed is unfamiliar.

Are some doctors unfairly influenced by the pharma industry?
It is perfectly acceptable for a pharma company to market its products among the medical fraternity. Medical representatives are trained to detail doctors about the company’s brands, after discussing pertinent scientific literature.
However, as is the case in every profession, there are some dishonest individuals in the doctor community too, who engage in writing prescriptions in return of special favours and illegal incentives by the pharma company. Though this predominantly involves smaller and relatively unknown firms that resort to unethical means to gain market hold, larger companies are no exception. Fortunately, this is a fading trend: compared to two decades ago.
However, this is not a valid reason to ask doctors to completely switch to writing generic names. Simply by transferring the privilege of choosing the brand from the doctor to the medical shop staff, only the venue of potential corruption is being shifted, not eliminated.
A doctor would never want his patient not to feel better. Once he discovers certain medications are substandard, it is impossible that he will continue to prescribe those. Apart from being against medical ethics, it is not healthy for his or her long-term practice either, as poor feedback from existing patients will scare future patients away. Thus, there is a certain self-limiting property to the alleged wrongdoing by the above minority of doctors.
In contrast, the person who dispenses medicine at the pharmacy has no such relationship with the patient as he or she is not a qualified medical practitioner. Besides, in India, this person is frequently an unqualified shop assistant who learned ‘on the job’- as opposed to a genuine pharmacist.
Whether the pharmacy dispenses a low-quality medicine or good-quality medicine, the doctor remains responsible for the outcome because of the doctor-patient relationship.
The scale of corruption concerning pharma and healthcare goes far beyond a few doctors that accept undue favours in return for preferring a certain brand. It ranges from adulteration of the raw material used in manufacture, diluting the product below all acceptable standards, manufacture and sale of counterfeit medications, demanding of unacceptably high margins for purchasing the product, obtaining fake inspection certificates in exchange of bribe, acceptance of low-quality tenders submitted by people of special interest, unacceptable storage practices such as switching off the refrigerators at night to save money, storing medicines at unacceptably high temperatures resulting in product degradation, to tampering with the expiry date by erasing the original date using spirit and cotton – just to name a few.
Critically analysing the above list of wrongdoings from the patient’s perspective, while the doctor’s preference of a particular brand is unlikely to result in direct harm, all of the others could cost patients their health, and sometimes their life.
What about the role of pharma industry in sponsoring doctors’ meetings?
Incidentally, the role of pharma companies in sponsoring academic conferences for doctors has been questioned by some quarters. Reputed pharmaceutical firms, often collectively, do help in organising academic conferences (CME programs, or continuing medical education) for doctors. Such meetings are an important medium of updating medical knowledge for doctors who are otherwise busy with clinical work.
The topics chosen for these programs are of the highest quality scientific content – and have nothing to do with the sponsoring companies or their products. In a world of fast-paced medical progress, such CME programs are in fact a service to the community by the pharma industry, as the scientific knowledge gained by each doctor is of direct benefit to the next patient.
The only occasion where a company’s products are discussed are the occasional drug launch symposia that are hosted by pharma companies, each time a new product is released. Just as other industries invite potential clients for the launch of their products, whether it is a new car model or an apartment complex, these symposia serve to make doctors familiar with the new product, and are not to be confused with CME programs.
Why are developed countries using generic while India is not?
It is true that over 85% of medicines dispensed in countries like the US are in the generic category. This is because the US FDA has stringent quality control measures including bioequivalence testing which ensures that just the right amount of medication with the desired effect is contained in each tablet sold. In fact, some reputed pharma companies from India export generic medicines to the UK, US and elsewhere. Interestingly, thanks to the US FDA’s stringent requirements, some of these companies recently got delisted.

In India, there is much less quality control on manufacture of medication except perhaps among those recognized as GMP (Good Manufacturing Practice) companies. Manufacturing plants from the highest standard to the lowest can be found. While reputed companies manufacture their products (both branded and generic) in climate-controlled laboratories using state-of-the-art machinery operated by trained personnel who wear disposable masks and gloves, there are cottage industries that manufacture medicines in dark, damp and dirty warehouses - employing untrained staff who handle the medicines with their bare hands and violate every known standard of hygiene.
Such sub-standard units are located in rural areas and suburbs - including Bangalore, Pondicherry, Gujarat, Himachal Pradesh, Jammu and Kashmir to name a few; their nefarious activities have been brought to light by several media sting operations recently. Several of their products are also being sold as generic medicine.
It is thus not possible to equate the quality of a tablet produced in a facility with international quality standards, to a similar-looking pill made by such shady establishments.
At this point, in the absence of consistently good-quality generic medicine in India, it is no wonder that doctors prefer to write the brand of medicine they can trust.
What is the current status of medication quality testing in India?
In Kerala, out of approximately 250,000 batches of medicines produced every year, only about 6000 are able to be tested by the existing infrastructure and personnel. The state has only two drug testing labs and less than half the recommended number of drug inspectors in active service at this time, with several posts still lying vacant.
Several government hospitals in India stock medications based on the lowest priced tender. Such brands need not always be of acceptable standard; many of these products have historically failed subsequent drug quality testing. However, by the time the test results become available, these batches of medicine would have sold out.
As existing drug-testing mechanisms are inadequate, unfortunately the only readily available benchmark of quality remains the doctor’s past experience with the product.
When asked why they always selected the lowest priced tender of medicines to stock in the pharmacy, doctors in government service responded that if they chose a more expensive brand, they could be subjected to allegations of corruption, even though the selection of brand was based on merit alone. Not only does this amount to unwarranted harassment for the already overworked doctor, it also delays the medication purchase till the due process is through.
In fact, a significant number of patients who visit government hospitals prefer to purchase their medicines from private pharmacies outside, in a hope that they would receive better quality drugs.
Counterfeit medicines are a worldwide problem, and published reports indicate that 5-25% of medicines available in India are either fake or of substandard quality. With a population of 1.3 billion, this translates to enormous numbers of patients taking poor quality medicine.
The doctor’s dilemma
In India, the vast majority of doctors therefore prefer to write a brand name that they can trust, so that they are sure that the patient receives the intended medication at the right dose. This trust was gained through years of practice, and from the feedback of thousands of patients. It is through such follow-up that doctors decide which brands really work and which ones don’t.
Doctors often deal with life-threatening conditions such as pneumonia, sepsis, multisystem failure and worsening of asthma. The doctor cannot afford to try out unknown brands of medication that he or she is not sure would work. In such situations, they always fall back to the most reliable makers of medications, trusting their quality standards.
If the manufacture of all medications in India was brought under a high-quality umbrella, then doctors would have no hesitation to write just the generic name on the prescription. Although the government is now providing GMP certification to pharma firms that meet certain quality benchmarks, a universal seal of quality similar to the ISI - which cannot be forged - should be ideally present on each batch of medication.
What does the patient want?
It is not the doctor, the pharmacist, the drug inspector, the government or the manufacturer - the patient is the most important person in this context. From the patient’s perspective, the reason for going to the doctor is to get relief from suffering. The patient trusts the doctor to rely on his or her knowledge, skills and past experience to diagnose the illness and prescribe the right remedy, which frequently involves tablets.
In Indian culture, the doctor-patient relationship is quite unique, and some attribute a spiritual element to it. Several patients consider the doctor a manifestation of God, and it is such steadfast faith that in fact helps them cope with many illnesses. From this standpoint, in India, the patient places a lot of value and trust specifically in the doctor’s written prescription.
Most patients are now aware that there is considerable variation in quality between brands, and feel that if the privilege of choosing the brand is taken away from the doctor and given to the pharmacy staff member, they would not have absolute trust in taking the medication dispensed. If the patient takes a medication without complete trust, it is unlikely that it will work.
In India, over 70% patients pay out-of-pocket for medical expenses, as there is no universal health insurance coverage. Thus, cost of medication remains a problem for patients, particularly for older people who frequently carry long lists of medications. For them, even the price difference of a few paise per tablet will amount to substantial savings long-term. This is because their earning capacity weakens in old age, and the net value of their savings or pension gets diminished by inflation.
While the well-to-do patient might not care too much about the price of the brand prescribed, this might not be the case for someone with limited financial reserve; many of them would rather have a cheaper substitute. Such patients suffer when their doctor chooses relatively expensive brands.
If the medication is of poor quality, the patient’s illness worsens, leading to prolonged courses of treatment, at times developing complications of disease or side effects from overdose. When they fail to get better, many patients turn towards unscientific and unauthorised treatments, falling victim to quackery which is widespread in India. In spite of there being a Drugs and Magical Remedies Act that prohibits quackery, fast-talking quacks operate freely in India, making claims of miracle cures and charging as they please, taking unsuspecting patients into confidence. They thrive by word-of-mouth largely generated by their own henchmen, as well as by sleazy ads that appear in the back columns of newspapers and other media.
On the good side, many doctors are cost-conscious and empathetically write more economical choices of good-quality drugs for those who cannot afford. Several hospitals including the private sector do offer discounted rates for patients of limited paying capacity. At the doctor’s request, many pharma companies offer direct discounts to patients who have difficulty affording long-term medications. Unfortunately, such well-intentioned programs are sometimes misinterpreted by the public.
The Government of India has launched the Jan Oushadhi chain of outlets where generic medicines are available at low cost. Several essential drugs have been brought under the umbrella of price control already, thanks to the Drugs Price Control Order of 2013. Conscientious doctors try to trim non-essential medications from long lists, in the best interest of the patient. More on this topic was discussed in my earlier article ‘How to make the most out of a doctor visit’.
In summary, switching to generic prescribing in India might sound good on paper, and could even work in a few selected centres, but is otherwise impractical and counterproductive at multiple levels.

Doctors earnestly want their patients to get better, and prescribe the most reliable medication in their experience for that. Such knowledge comes from years of clinical practice, and feedback from patients.
Shifting the choice of brands from the doctor to the medical shop staff will greatly worsen the chance of unethical doings, as there is no control on which brand gets dispensed at the sales counter. Patients will suffer from receiving low-quality medications dispensed with profit margin as the benchmark, instead of quality and effectiveness.
In a country where the quality of medications manufactured and sold cannot be assured, asking doctors to write only the generic name on a prescription is like asking someone to drive a train before laying the railway tracks first. As in developed countries, doctors in India too are willing to prescribe in generic format, but only at a time when all available medications in the country are of the same manufacturing standard, verifiable by a non-forgeable government seal of quality.
Further reading
The FDA’s Q&A about generic medicines.
Growing threat from counterfeit (fake) medicines: WHO paper
WHO paper on SSFFC (Substandard, spurious, falsely labelled, falsified or counterfeit) medicines
What does a tablet contain? What are fillers or excepients?
Counterfeit medicines in India.
The prevalence of substandard medicines in India
Shortage of drug inspectors in India.
How to make the most out of a doctor visit? Article by Dr Rajeev Jayadevan
What are medication side effects? Article by Dr Rajeev Jayadevan
Why medicines are expensive in India, despite lower cost of production.
Drug price control order of 2013
The author is a senior consultant gastroenterologist and deputy medical director, Sunrise group of hospitals)


























