Jyoti, a 32-year-old movie buff and mother of two, was frantic after hearing the news of actor Sridevi's sudden death. She was concerned whether she was at risk for a heart attack. She checked the internet and decided to get a treadmill test, and then consulted a cardiologist. Even though she felt healthy, Jyoti reckoned it was better to ‘do the test’ and ‘make sure that everything is okay’, rather than be caught by surprise by a heart attack.
The cardiologist was not impressed by her demand for an exercise stress test. “You don’t need a stress test” he declared, much to Jyoti’s disappointment.
“But why, doctor?” asked Jyoti. “I read on the internet that a treadmill test can pick up heart disease in early stages, while it is still treatable! Why wait for a heart attack?”
The doctor explained that Jyoti’s pretest probability for heart disease was low, and therefore the positive predictive value of the test would be unacceptably low, making the test no better than tossing a coin.
“Tossing a coin? I thought the test was pretty good to diagnose heart disease. What do those terms mean, doctor?” asked Jyoti.
This article is being written mainly to explain how the accuracy of any test can vary enormously based on the clinical profile of the patient, and to discuss the treadmill test in some detail.

How do heart attacks happen?
Most heart attacks, also known as myocardial infarction, happen when blood flow through the coronary arteries gets blocked. Coronary arteries are those arteries that supply the heart, carrying oxygen to the cardiac muscles. Perhaps the only muscles in the body that work non-stop till our death, the cardiac muscles require plenty of oxygen as fuel.
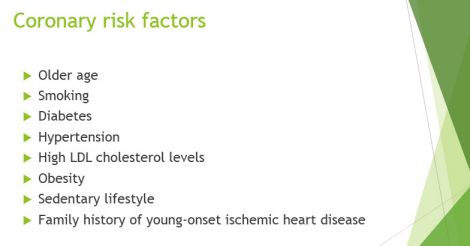
As people get older, these coronary arteries can become narrow due to a process called atherosclerosis. Plaques start building up along the walls of the arteries, particularly in those who smoke and those who are diabetic. As the plaques get bigger, the lumen gets narrower. In most cases, this process is silent—without any symptoms.
However, when blood flow is over 90% decreased, the heart muscle’s demands can no longer be met, and it starts sending pain signals as it starts to choke without oxygen. The pain becomes prominent when the heart muscles do extra work, for instance, while climbing a flight of stairs or walking up a slope. This is called angina, which typically happens at exertion and goes away with rest.
Sometimes, a plaque can rupture along the wall of the coronary artery, causing blood to clot at that site. Just as even a single car can completely block a narrow road, blood flow abruptly stops in the already narrow artery. This leads to injury to the heart muscle. This is termed a myocardial infarction, or heart attack.
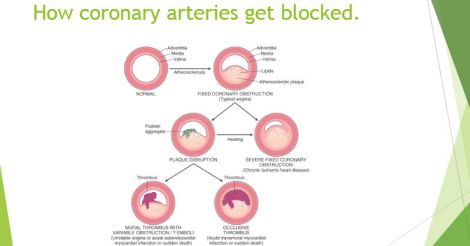
Are all arterial blocks dangerous?
No. In fact, most adults will develop some degree of atherosclerosis of their coronary arteries with advancing age. The vast majority of these do not cause heart attacks. Heart attacks occur either when the vessel becomes severely blocked as a result of progressive atherosclerosis, or when a plaque ruptures and causes blockade.
It is impossible to predict whether a mild block in the artery will progress into a heart attack in the future—chances are, it won’t. Hence, diagnosing a mild block in a person who is otherwise healthy and without symptoms is of questionable benefit at this time.
Over the past three decades, researchers have been studying an entity called ‘vulnerable plaque’, which is essentially an innocent-looking plaque, but could rupture suddenly causing a heart attack. As most of these plaques do not severely block the cavity of the artery, they are commonly missed by treadmill testing, or deemed insignificant by coronary angiograms.
In other words, even if someone has a normal #TMT or unremarkable coronary angiogram recently, that person could still develop a heart attack later if a vulnerable plaque ruptures suddenly.
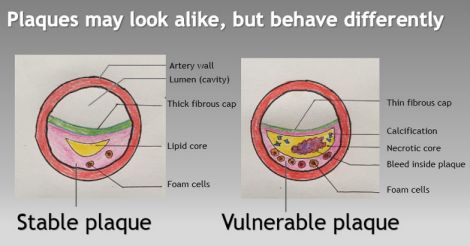
In contrast, the discovery of a severe block—typically occluding >70% of the lumen—will be helpful for the patient because corrective measures can be undertaken, with proven benefit. Stents (angioplasty) and bypass grafting (CABG) are the two most commonly used methods to treat such severe blocks.
Deploying a stent is like unfolding a tiny umbrella inside the blocked artery to blow it open. This is done by passing a catheter through the arteries—and does not require surgery.
CABG involves surgically replacing the diseased coronary arteries with healthy blood vessels harvested from other parts of the body. These treatments reduce the patient’s risk of developing heart problems in the future.
Although they are not of much use in identifying the smaller vulnerable plaques, TMT and coronary angiograms are good at detecting severe blocks.

How does TMT (treadmill test) work?
Let us imagine a patient who has a moderate coronary arterial block, where 70% of the lumen is obstructed. The blood flow at rest, although diminished, is adequate for the heart that is working at a relaxed pace. Therefore, if we hook up an ECG monitor, it will deliver a perfectly normal pattern.
Now let us turn on the treadmill and ask him to walk faster and faster. As the heart begins to work harder, the partially blocked artery is not able to supply the extra blood required for the task. As a result, the heart muscle supplied by that artery is starved for oxygen. The ECG leads pick up the distress signals sent out by the choking heart muscle—this helps the doctor diagnose ischemia. As the treadmill slows, these changes go away as the heart muscle’s oxygen demand comes back to baseline.
Thus, in a person with significantly blocked coronary arteries, the ECG displays certain typical abnormal patterns when ischemia is provoked by exercise. Hence the name exercise stress test (EST) or treadmill test (TMT) as it is popularly known.
In contrast, a person with healthy coronary arteries maintains a normal ECG pattern despite higher workload for the heart during the treadmill test.
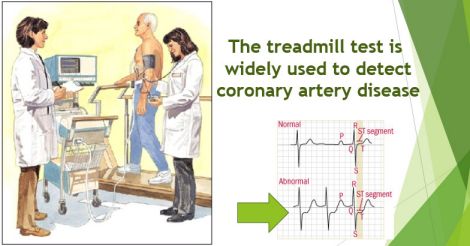
What is the role of a treadmill test (TMT) in clinical practice?
All over the world, the treadmill test is the most commonly used test to check for partially blocked coronary arteries. It is cheap, relatively safe and widely available. Variations of this test exist for those who cannot perform exercise; but are beyond the scope of this article.
Once the TMT is positive, the patient typically proceeds to undergo the gold standard test, which is a coronary angiogram. This is an invasive procedure carried out under X-ray guidance, where a thin catheter is introduced into the coronary arteries and a dye is injected to study the anatomy. If blocks are confirmed, they can be treated in the same sitting by deploying stents that ply them open.
What are the limitations of the TMT? Why not proceed directly with an angiogram instead?
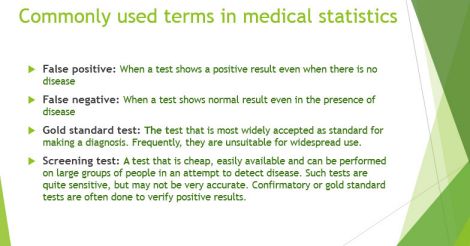
Like any other test, TMT also has its share of inaccuracies. In some cases, the test may be false positive, which means that it will say there is disease when in fact there is none, while in other instances it becomes false negative, where the test remains negative in spite of significantly blocked coronary arteries.
The problem with the test being false positive is that it leads to unnecessary coronary angiograms, which involve radiation as well as several other complications including allergic reactions, kidney damage, bleeding and stroke, although the risk is small (0.1 % - 0.01%). Unlike TMT which is generally safe, the side effect profile of the coronary angiogram makes it unsuitable as a general screening test. Other options such as CT coronary angiogram and CT calcium scoring are beyond the scope of this discussion.
Those patients who are given a false positive verdict on TMT could experience severe anxiety from needless fear of heart disease, when in fact there is none. Even after subsequent testing, it could become hard to convince some patients otherwise; the shadow of doubt still lingering can lead to significant mental stress.
How accurate is the TMT?
The methods to measure the accuracy of any test were elaborately explained in my earlier article.
The overall sensitivity of the TMT is 68%, which means that when done on 100 people with significant heart disease, the test can correctly identify 68 of them, while being false negative in 32.
The specificity of the test is 72, which means that if performed in a hundred people in good health, the test will correctly remain negative in 72, while turning false positive in 28.
The sensitivity of the TMT can vary from 50-85% depending on the number and the severity of the blocks being studied. For instance, if the test is performed exclusively on a group of patients with triple vessel disease, it is more likely to be positive, which would theoretically mean higher sensitivity. But in real life, it is not practical to expect all patients undergoing a test to have exactly the same pattern and extent of disease. Thus, sensitivity and specificity of a test are theoretical parameters that are measured in ideal situations.
What is a better way to determine the practical accuracy of a test?
In real life, the accuracy of the test is better determined by the positive predictive value (PPV), which estimates the ability of the test to diagnose disease using another parameter: if we take a hundred positive TMT reports, how many of these will actually have underlying heart disease?
Unlike sensitivity and specificity that solely represent the test, PPV applies to the actual patients on whom the test is performed. From a practising doctor’s standpoint, PPV reflects real-life clinical situations.
For instance, let us imagine a doctor ordering a test to diagnose heart disease on patients who visit him that day. Positive predictive value is basically about the doctor looking back at all the positive test results at the end of the day, and asking how many of those with positive test results actually had heart disease. This parameter is of great practical value to both the doctor as well as the patient.
How can the same test be accurate as well as inaccurate in various clinical settings?
A seldom-recognised fact about clinical testing is that the positive predictive value of the test varies hugely depending on the prevalence of the disease in the community being studied. Prevalence is essentially how common the disease is in a group of people. It is also known as pre-test probability, which means how likely the patient is to have the disease in question.
Given the sensitivity (68%) and specificity (72%) mentioned above, if this test is performed in a group of people where the prevalence of heart disease is 1 in 100, then the PPV is only 2%, which means that out of a hundred positive TMT results, only two will actually have heart disease!
Now let us perform this test in a population where the prevalence is higher at 1 in 10. The PPV rises to 20%, which means that out of 100 positive test results, only 20 will actually have heart disease. Importantly, the remaining 80% will NOT have heart disease on angiogram.
If we do the same test in a group of people where the prevalence of heart disease is 1 in 2 or 50%, then the PPV will rise to 70%, which means that a positive test indicates a 70% likelihood of actually having heart disease.
Scarface: illustration of PPV using a hypothetical non-medical example
For a learning experiment, let us use the presence of a ‘scar on the face’ as a screening test to identify whether a person has a background of violent crime. The rationale here being the commonly held view that a person who engages in acts of armed assault is more likely to have a scar on the face than other people.
If a person has a large scar on his face, the test shall be considered positive, and a confirmatory test is then ordered. In this case, the confirmatory test (gold standard) is that person’s police records. If the records show he had committed a violent crime in the past, then the test result is a true positive.
However, if that person’s records show that he never committed such a crime in spite of having a scar, then the result is false positive.
In people with no scar, the test is deemed negative or normal.
Now that the terms are laid out, let us try out the math experiment.
Let us first apply this test in a shopping mall. Out of 1000 people who visit the mall, let us imagine we identified ten people with a scar on their face. What are the chances that the test correctly identified a criminal? Most likely, none of the apparently ‘positive’ tests would have identified a criminal. The reason is because these ten people could have got a scar through other means than violence or assault. Thus, all 10 test positive results are called false positive, yielding a positive predictive value of zero. In other words, the above test is of no discriminating value in such a setting.
Now, let us perform the same test in a different study population, that is among 1000 inmates of a state prison. The test turns positive on 10 people in that population, and we then verify their records to confirm or refute the diagnosis. We discover that 7 of them had in fact committed violent crime in the past (true positive), while 3 had not engaged in violent criminal activity. These three (30%) are considered false positive. Therefore, this test had a 70% positive predictive value in this setting (7 out of 10 were correct).
The difference between the two scenarios here is the prevalence or pre-test probability. When the same test was applied in a prison setting with high prevalence, it correctly identified several cases, while it failed completely in a low-prevalence setting such as a shopping mall.
In this experiment, we proved that just a change in the setting improved the positive predictive value of the exact same test from zero to 70%.
Thus, the ability of a test to correctly identify disease depends on how common the disease is in the study population.
How does this apply to Jyoti’s case?
Coming back to the example of Jyoti described above, at the age of 32 and without any cardiac symptoms or significant risk factors such as smoking, diabetes or positive family history, the pre-test probability of heart disease is miniscule, perhaps less than 1 in 1000, which means that even if she got a positive test report, it would be wrong (false positive) over 99% of the time.
The big question before ordering any test is whether it will change (improve) the doctor’s management of the patient. In the case of the low-risk adult without symptoms, studies have shown that doing a resting ECG or treadmill testing will not significantly change the treatment.
The general advice for prevention of heart disease is the same for everyone—and does not depend on the outcome of such tests. Put another way, if it is already raining outside, we don’t need to consult a weather channel to decide whether or not to carry an umbrella.
The cardiologist knew this—and did not want to subject Jyoti through unnecessary testing, which could have led to unwarranted angiograms and mental aggravation that would follow a positive test report. Hence, he advised Jyoti not to undergo the test and to simply follow a healthy lifestyle.
Who really needs the TMT then?
With rare exceptions, the treadmill test is to be done only among those with intermediate or high pre-test probability of heart disease. For example, in an older person with chest pain and multiple coronary risk factors, the test may be performed with considerable accuracy to detect heart disease. Unlike the case of young healthy adults with no risk factors, doing the stress test in such patients can result in a significant number of meaningful treatment decisions and interventions.
In situations where the pre-test probability is very high or certain, the cardiologist might proceed directly to an angiogram (the gold standard test) without the need of a TMT.
Why did Jyoti demand a stress test? What are the problems with internet self-diagnosis?
The human mind can easily be biased—after all, it is not a machine. It is therefore natural to become concerned when someone whom we know is unexpectedly diagnosed with heart disease or cancer. However, that doesn’t always mean that we would develop the same disease. Almost invariably these are random events, and exceptions don’t define reality. When in doubt, it is better to consult the doctor rather than jump into conclusions or engage in self-directed testing.
Unlike the west, in India, patients commonly refer themselves directly to the specialist. Cardiologists frequently encounter patients who check the internet, diagnose themselves with a problem and then demand the doctor to perform tests to confirm the diagnosis. The fallacies of internet self-diagnosis were elaborated in my earlier article “Google vs. Doctor; why internet self-diagnosis is a bad idea”
In summary, clinical tests are not 100% precise all the time. Their accuracy depends on the pre-test probability that can be estimated by the treating physician. In other words, tests are only to be ordered in the right context by a qualified doctor after studying the patient’s history.
If performed on people with low pre-test probability, there will a high percentage of false-positive tests—and patients will end up doing a large number of unnecessary confirmatory tests. This will not only be expensive, but also cause mental aggravation, besides exposing the patient to side effects of subsequent tests. Asymptomatic young women without cardiac risk factors are at very low pre-test probability of heart disease; hence doing the TMT in this group serves almost no purpose.
The principle of Positive Predictive Value applies to all clinical investigations including blood tests and scans—not just the treadmill test.
Further reading
1. The science behind a lab test.
2. How to calculate sensitivity, specificity and positive predictive value
3. The basics of the exercise stress test.
4. The US preventive services task force (USPSTF) recommends against routine exercise stress testing.
6. Sensitivity and specificity of treadmill testing: Hurst’s The Heart, manual of cardiology
7. Exercise ECG testing: Braunwald’s Heart Disease, a textbook of cardiovascular medicine, 11th edition
8. Why the internet is not a good way to diagnose disease.
(The author is a senior consultant gastroenterologist and deputy medical director, Sunrise group of hospitals)
Read more: Latest in Health


























 Treadmill
Treadmill